Outbursts in Autoimmunity: Disease Flare-ups

Unpredictable and disruptive, autoimmune disease flare-ups can throw a wrench in your plans.
Discover the answers to some of the following questions in our article:
What are the potential causes and triggers for autoimmune flare-ups?
What is happening in the body when flare-ups occur?
What flare-ups typically occur in common autoimmune diseases?
What Are Autoimmune Disease Flare-Ups?
Also known as bouts, relapses, or episodes, autoimmune disease flare-ups occur when patients show a dramatic worsening of disease signs and symptoms or when they develop new ones. These manifestations occur in one or more organs of the body, are usually more severe than symptoms regularly observed in autoimmunity, and often interfere with daily activities.
Distinguishing between a flare-up and a regular symptom may be difficult.
Triggers, Body Responses, and Symptoms
Flare-ups are markers of autoimmune disease activity, meaning that the signs or symptoms can usually be observed or measured in an organ or organ system. Factors that spur autoimmune disease flare-ups include stress, diet, drugs, pregnancy, changes in microbial populations, and seasonality (1, 2).
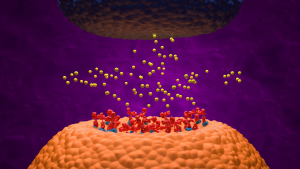
During a flare-up in autoimmune diseases, such as arthritis or lupus, a person’s immune system attacks the body, leading to signs and symptoms. More specifically, these bouts are triggered by autoantibodies, specialized cells known as B and T cells, and cellular pathways that involve substances called cytokines which cause inflammation in different tissues and organs (3, 4, 5).
Common flare-up symptoms include depression, exhaustion, unusual rashes, poor sleep, fever, and increased pain. However, different autoimmune diseases feature specific bouts that often depend on the body sites they affect.

Systemic Lupus Erythematosus (SLE) Flare-Ups
During SLE flare-ups, people may either experience a return of regular symptoms or develop new ones. Triggers include emotional stress, surgical procedures, injury, and pregnancy (6). The episodes are caused by autoantibodies that attack healthy tissue, leading to tissue inflammation and damage (5). Fever, joint pain, increased fatigue, and rashes are common symptoms, and gastrointestinal complications may also occur.
Nephritis, caused by inflammation of the kidneys, is one of the most severe flare-ups of SLE, with up to 20% of patients with SLE nephritis developing end-stage renal disease (7). Pregnant women with SLE and a history of kidney disease are at risk for flare-ups that may lead to pre-eclampsia, preterm birth, and fetal death (8). High-intensity immunosuppressive therapy followed by longer courses of less intensive therapy is often prescribed to control disease activity of life-threatening lupus flares and prevent relapses (9). However, drug administration should be closely monitored during pregnancy and lactation.
Some SLE flare-ups may occur without clinical manifestations, so patients should be regularly screened by a physician for signs and symptoms.

Multiple Sclerosis (MS) Flare-Ups
Relapsing remitting multiple sclerosis (RRMS) is a type of MS marked by flare-ups caused by stress, infections, medical procedures, older age, and heat exposure. The flare-ups can be mild to severe, depending on which areas of the central nervous system are affected (10). Symptoms include limb weakness, blurred vision, slurred speech, numbness, bladder issues, and memory and concentration problems.
One way to distinguish between RRMS flare-ups and regular symptoms is to look at their duration and pattern (10, 11). A symptom is considered a flare-up when it has lasted for at least 24 hours, though they typically last longer (sometimes for weeks or even months at a time). Flare-ups usually occur at least 30 days after an earlier bout (10).
Although flare-ups may clear on their own, medications such as corticosteroids and immunosuppressants are needed in more severe cases. Physical therapy may be recommended to regain strength. Minocycline, a tetracycline antibiotic, has shown promise for treating RRMS (12).

Other Autoimmune Disease Flare-Ups
Autoimmune disease flare-ups can also affect the liver and skin.
Psoriasis features skin flare-ups that alternate with periods of remission. Common triggers include medications, stress, cold weather, alcohol intake, and trauma to the skin (13, 14). When a person’s mild lesions become painful and inflamed, a flare-up is probably occurring. In addition to topical, oral, and light therapies, mindfulness and meditation were recently found to be useful in managing psoriasis episodes (15).
A more rare disorder, autoimmune hepatitis, is characterized by the infiltration of T cells in the liver and a high risk of relapses (16). The disease classically affects women of reproductive age and is known to cause especially serious and unpredictable liver flare-ups in pregnancy, leading to pre-term birth and interfering with proper fetal growth (17). Multidisciplinary surveillance and close evaluation of pregnant women with autoimmune hepatitis flare-ups has led to better outcomes (17).
Living Well With Flare-Ups
Recognizing flare-ups in autoimmune disease can be difficult and take trial and error, but it is essential for managing any condition. Patients should consult their primary care physician or specialists when experiencing changes in regular autoimmune symptoms, especially if daily activities are affected. Exercising, eating well, resting, practicing mindfulness, and eliminating flare-up triggers will complement any therapy, but major lifestyle changes or switches in treatment should be discussed with a healthcare provider.

About the Author
Damiana Chiavolini, MS, PhD is a freelance writer who specializes in medical and life science topics. As a trained researcher, she authored journal articles in the areas of infection and immunity and wrote booklets and book chapters about different diseases. As a professional communicator, she writes feature articles for magazines and other publications and produces content for higher education platforms. Damiana is also an experienced academic editor, microbiology educator, writing coach, and fragrance blogger. She is a contributing member of the American Medical Writers Association and the current president of the association’s Southwest chapter.
Sources
- Article Sources
Mousa, W. K., Chehadeh, F., & Husband, S. (2022). Microbial dysbiosis in the gut drives systemic autoimmune diseases. Frontiers in immunology, 13, 906258. https://doi.org/10.3389/fimmu.2022.906258
Watad, A., Azrielant, S., Bragazzi, N. L., Sharif, K., David, P., Katz, I., Aljadeff, G., Quaresma, M., Tanay, G., Adawi, M., Amital, H., & Shoenfeld, Y. (2017). Seasonality and autoimmune diseases: The contribution of the four seasons to the mosaic of autoimmunity. Journal of autoimmunity, 82, 13–30. https://doi.org/10.1016/j.jaut.2017.06.001
Chang, M. H., Levescot, A., Nelson-Maney, N., Blaustein, R. B., Winden, K. D., Morris, A., Wactor, A., Balu, S., Grieshaber-Bouyer, R., Wei, K., Henderson, L. A., Iwakura, Y., Clark, R. A., Rao, D. A., Fuhlbrigge, R. C., & Nigrovic, P. A. (2021). Arthritis flares mediated by tissue-resident memory T cells in the joint. Cell reports, 37(4), 109902. https://doi.org/10.1016/j.celrep.2021.109902
Jenks, S. A., Cashman, K. S., Woodruff, M. C., Lee, F. E., & Sanz, I. (2019). Extrafollicular responses in humans and SLE. Immunological reviews, 288(1), 136–148. https://doi.org/10.1111/imr.12741
Thanou, A., Jupe, E., Purushothaman, M., Niewold, T. B., & Munroe, M. E. (2021). Clinical disease activity and flare in SLE: Current concepts and novel biomarkers. Journal of autoimmunity, 119, 102615. https://doi.org/10.1016/j.jaut.2021.102615
Lupus Foundation of America. What is a lupus flare? https://www.lupus.org/resources/what-is-a-flare
Alforaih, N., Whittall-Garcia, L., & Touma, Z. (2022). A Review of Lupus Nephritis. The journal of applied laboratory medicine, 7(6), 1450–1467. https://doi.org/10.1093/jalm/jfac036
Dao, K. H., & Bermas, B. L. (2022). Systemic Lupus Erythematosus Management in Pregnancy. International journal of women’s health, 14, 199–211. https://doi.org/10.2147/IJWH.S282604
Fanouriakis, A., Tziolos, N., Bertsias, G., & Boumpas, D. T. (2021). Update οn the diagnosis and management of systemic lupus erythematosus. Annals of the rheumatic diseases, 80(1), 14–25. https://doi.org/10.1136/annrheumdis-2020-218272
Healthline. Understanding multiple sclerosis (MS) flare-ups. https://www.healthline.com/health/multiple-sclerosis/exacerbation-ms-attack
Leray, E., Moreau, T., Fromont, A., & Edan, G. (2016). Epidemiology of multiple sclerosis. Revue neurologique, 172(1), 3–13. https://doi.org/10.1016/j.neurol.2015.10.006
Marchand, D. K., & Butcher, R. (2019). Minocycline for Relapsing-Remitting Multiple Sclerosis and Clinically Isolated Syndrome: A Review of Clinical Effectiveness and Guidelines. Canadian Agency for Drugs and Technologies in Health. https://pubmed.ncbi.nlm.nih.gov/31721547/
Gregoire, A. R. F., DeRuyter, B. K., & Stratman, E. J. (2021). Psoriasis Flares Following Systemic Glucocorticoid Exposure in Patients With a History of Psoriasis. JAMA dermatology, 157(2), 198–201. https://doi.org/10.1001/jamadermatol.2020.4219
Rousset, L., & Halioua, B. (2018). Stress and psoriasis. International journal of dermatology, 57(10), 1165–1172. https://doi.org/10.1111/ijd.14032
Bartholomew, E., Chung, M., Yeroushalmi, S., Hakimi, M., Bhutani, T., & Liao, W. (2022). Mindfulness and Meditation for Psoriasis: A Systematic Review. Dermatology and therapy, 12(10), 2273–2283. https://doi.org/10.1007/s13555-022-00802-1
Cardon, A., Conchon, S., & Renand, A. (2021). Mechanisms of autoimmune hepatitis. Current opinion in gastroenterology, 37(2), 79–85. https://doi.org/10.1097/MOG.0000000000000704
Braga, A., Vasconcelos, C., & Braga, J. (2020). Autoimmune hepatitis and pregnancy. Best practice & research. Clinical obstetrics & gynaecology, 68, 23–31. https://doi.org/10.1016/j.bpobgyn.2020.03.007