How Autoimmune Disease Affects Fertility

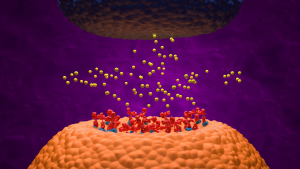
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own healthy cells and tissues, leading to chronic inflammation and organ damage. This immune overactivity can affect fertility in several ways.
Chronic inflammation may lower sperm and egg counts, trigger early menopause, or create an inhospitable environment for pregnancy. Autoimmunity can also interfere with the hormones needed for reproduction, cause blood clots in the placenta, or increase the risk of miscarriage and stillbirth.
“If a patient has an autoimmune disease and has been trying for longer than six months, both partners need to be evaluated,” said Dr. Cuoghi Edens, a rheumatologist and assistant professor of internal medicine and pediatrics at the University of Chicago Medicine.
What Is Infertility?
Infertility is defined as the inability to conceive after one year of regular, unprotected sex if under age 35. It affects up to 15% of couples worldwide, with male and female factors contributing about equally.
According to Dr. Edens, infertility is often multifactorial:
“There are specific issues that affect males and females separately in regard to their ability to procreate, such as problems with the sperm or egg, anatomy of their reproductive organs, or hormonal issues,” she said. “For example, a male may have a low sperm count, but his partner could have blocked fallopian tubes or endometriosis.”
This is in addition to any other diagnoses they may have or medications that could affect their fertility. Infertility can manifest in many ways, including difficulty with conception, implantation, and pregnancy maintenance, as well as recurrent miscarriages and stillbirths. Social and cultural factors also play a role, including access to healthcare, stigma, and societal pressure around childbearing.
Autoimmune Diseases Linked to Infertility
Autoimmune diseases can cause infertility in both males and females.
As a rheumatologist, Dr. Edens sees firsthand that women with systemic lupus, rheumatoid arthritis, juvenile arthritis, psoriatic arthritis, Sjögren disease, mixed connective tissue disease, and other rheumatic diseases can have a hard time becoming pregnant or staying pregnant. Males with these diagnoses can also struggle to father a child, although less often.
Systemic Lupus Erythematosus (SLE)
SLE affects the immune system and can cause infertility in women by prematurely decreasing the number of eggs. Treatment for SLE can cause damage to the ovaries that leads to ovarian failure. Some women also have clotting issues with SLE, which increases the risk of miscarriages and stillbirths. In men, SLE can cause erectile dysfunction or inflammation that damages the testicles and reduces sperm count.
Rheumatoid Arthritis (RA)
Women with RA have been found to have a higher risk of infertility compared to the general population, which may be due to hormonal imbalances, ovulatory dysfunction, or the fact that women with RA may delay becoming pregnant due to their diagnosis or its medications. The main medication used to treat RA, Methotrexate, is not safe for pregnancy. In men, RA can cause inflammation that damages the testicles and reduces sperm count.
Antiphospholipid Syndrome (APS)
APS is an autoimmune disease associated with recurrent miscarriages, stillbirths, and other pregnancy complications, which can ultimately lead to infertility. This is caused due to its impact on blood clotting. Specifically, the abnormal blood clots can affect the blood flow to the uterus, disrupting the normal development of the embryo or impairing the implantation of the fertilized egg. Adequate blood flow is crucial for a healthy pregnancy, as it ensures that the developing fetus receives the necessary nutrients and oxygen.
Autoimmune Thyroid Disease (AITD) / Hashimoto’s Thyroiditis
AITD is a common condition that can affect fertility in women by disrupting their hormonal balance. Insufficient levels of thyroid hormones, as seen in Hashimoto’s disease, can disrupt the menstrual cycle and ovulation.
Inflammatory Bowel Disease (IBD)
Crohn’s disease and ulcerative colitis can potentially impact fertility in several ways. Malnutrition due to the body’s poor absorption of nutrients from food may affect the body’s ability to support a healthy pregnancy. The corticosteroids and immunosuppressants used to manage the disease can have side effects that may interfere with fertility by affecting hormonal balance or have direct effects on reproductive organs. Other factors, such as chronic inflammation in the abdominal area, and surgical interventions, may also affect the function of the reproductive organs.
Celiac Disease
Celiac disease damages the lining of the small intestine, reducing the absorption of nutrients from food, including essential vitamins and minerals. Proper nutrition is crucial for reproductive health, and deficiencies caused by malabsorption can affect fertility. Hormonal imbalances also may interfere with the menstrual cycle, ovulation, and overall reproductive function. Chronic inflammation in the small intestine, a characteristic of celiac disease, can extend to other parts of the body, potentially affecting the reproductive system.
Type 1 Diabetes
Type 1 diabetes affects insulin levels and can lead to hormonal imbalances, disrupting the normal menstrual cycle and ovulation in women, and affecting sperm production in men. Diabetes can also damage blood vessels and reduce blood flow throughout the body, including those in the reproductive organs, which can impact their function and fertility. Diabetes can cause damage to nerves, potentially leading to difficulties in achieving or maintaining an erection in men and affecting sexual function in women. High blood sugar levels may also affect the quality of eggs, potentially making it more challenging to conceive. Women with diabetes may face a higher risk of complications during pregnancy, such as gestational diabetes and preeclampsia.
How Does Autoimmune Disease Interfere with Fertility?
“Our body is smart, so if it is inflamed or stressed, it knows that it is not a good time for pregnancy,” says Dr. Edens.
The ways autoimmunity contributes to infertility are not fully understood, but several broad mechanisms across different autoimmune conditions are known:
- Chronic inflammation lowers egg and sperm reserves
- Immune stress signals that suppress fertility during disease flares
- Premature ovarian insufficiency (POI) and early menopause in women, possibly from long-term inflammation
- Hormonal disruption that interferes with ovulation or sperm production
How Do Medications for Autoimmune Disease Affect Fertility?
In addition to the immune system itself, some autoimmune disease treatments can affect fertility.
- Cyclophosphamide – a chemotherapy agent used for severe rheumatic diseases; can cause permanent ovarian damage.
- Methotrexate – commonly prescribed for rheumatoid arthritis; unsafe in pregnancy and requires discontinuation before conception.
- NSAIDs – may temporarily impair ovulation or sperm production; effects are usually reversible after stopping.
- Sulfasalazine – can lower sperm counts; recovery may take up to three months after discontinuation.
- Steroids (e.g., prednisone) – may disrupt hormone signals that regulate ovulation and sperm formation.
Because of these effects, patients planning for pregnancy are often advised to review their medications carefully with their rheumatologist and reproductive specialist.
What Fertility Treatments Are Available for Those with Autoimmune Disease?
Yes, assisted reproductive technologies (ART) and other treatments can help, including:
- Intrauterine Insemination (IUI): Sperm placed directly into the uterus using a tube called a catheter.
- In Vitro Fertilization (IVF): Egg fertilized outside the body, embryo implanted into the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm injected directly into an egg during IVF. Often used when there are male factor infertility issues, such as low sperm count, poor sperm motility, or abnormal sperm shape.
- Third-Party ART: Use of donor sperm, eggs, embryos, or gestational surrogacy. Often used when one or both partners have fertility issues that prevent natural conception, or when there is a high risk of passing on a genetic disorder to a child. Persons with autoimmune diseases may also consider surrogacy if they have health conditions or take medications that are not compatible with pregnancy.
Other medical interventions for infertility include medication to stimulate ovulation, surgery to correct structural issues, and hormone therapy to balance hormone levels.
According to Dr. Edens, many patients who are infertile can benefit from an evaluation of why they are infertile and fertility treatments, and recommends this be done sooner than later, especially if over 35. However, it’s important to remember that the success rate for things like IVF and IUIs is still low and decreases as women age due to egg quality.
Sources
- Article Sources
Yatsenko, S. A., & Rajkovic, A. (2019). Genetics of human female infertility. Biology of reproduction, 101(3), 549–566. https://doi.org/10.1093/biolre/ioz084
Tabong, P. T., & Adongo, P. B. (2013). Understanding the social meaning of infertility and childbearing: a qualitative study of the perception of childbearing and childlessness in Northern Ghana. PloS one, 8(1), e54429. https://doi.org/10.1371/journal.pone.0054429
Richard A. Hickman, Caroline Gordon, Causes and management of infertility in systemic lupus erythematosus, Rheumatology, Volume 50, Issue 9, September 2011, Pages 1551–1558, https://doi.org/10.1093/rheumatology/ker105
Brouwer, J., Fleurbaaij, R., Hazes, J. M. W., Dolhain, R. J. E. M., & Laven, J. S. E. (2017). Subfertility in Women With Rheumatoid Arthritis and the Outcome of Fertility Assessments. Arthritis care & research, 69(8), 1142–1149. https://doi.org/10.1002/acr.23124
Backos, M., Rai, R., & Regan, L. (2002). Antiphospholipid antibodies and infertility. Human fertility (Cambridge, England), 5(1), 30–34. https://doi.org/10.1080/1464727992000199731
Thangaratinam, S., Tan, A., Knox, E., Kilby, M. D., Franklyn, J., & Coomarasamy, A. (2011). Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence. BMJ (Clinical research ed.), 342, d2616. https://doi.org/10.1136/bmj.d2616
Italian Group for the Study of Inflammatory Bowel Disease Working Group, et al. (2022). Female reproductive health and inflammatory bowel disease: A practice-based review. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver, 54(1), 19–29. https://doi.org/10.1016/j.dld.2021.05.020
Lasa, J. S., Zubiaurre, I., & Soifer, L. O. (2014). Risk of infertility in patients with celiac disease: a meta-analysis of observational studies. Arquivos de gastroenterologia, 51(2), 144–150. https://doi.org/10.1590/s0004-28032014000200014
Lin, Y. H., et al. (2018). Type 1 diabetes impairs female fertility even before it is diagnosed. Diabetes research and clinical practice, 143, 151–158. https://doi.org/10.1016/j.diabres.2018.07.010
American Society for Reproductive Medicine. (2015). In vitro fertilization (IVF).
American Society for Reproductive Medicine. (2018). Intracytoplasmic sperm injection (ICSI).
Centers for Disease Control and Prevention. (2024). About ART.