Autoimmunity and the Eyes: A Spotlight on Uveitis

The familiar quote: “The eyes are the window to your soul” (attributed to William Shakespeare) makes us think about sight as greater than the familiar 20/20 vision chart. Healthy eyes are essential to our well-being. Many with autoimmune conditions are challenged with secondary conditions or co-morbidities that accompany a primary condition. These conditions often contribute to significant health problems. Among the more rare and more serious conditions is uveitis, with approximately 30,000 new cases annually (1).
What Is Uveitis?
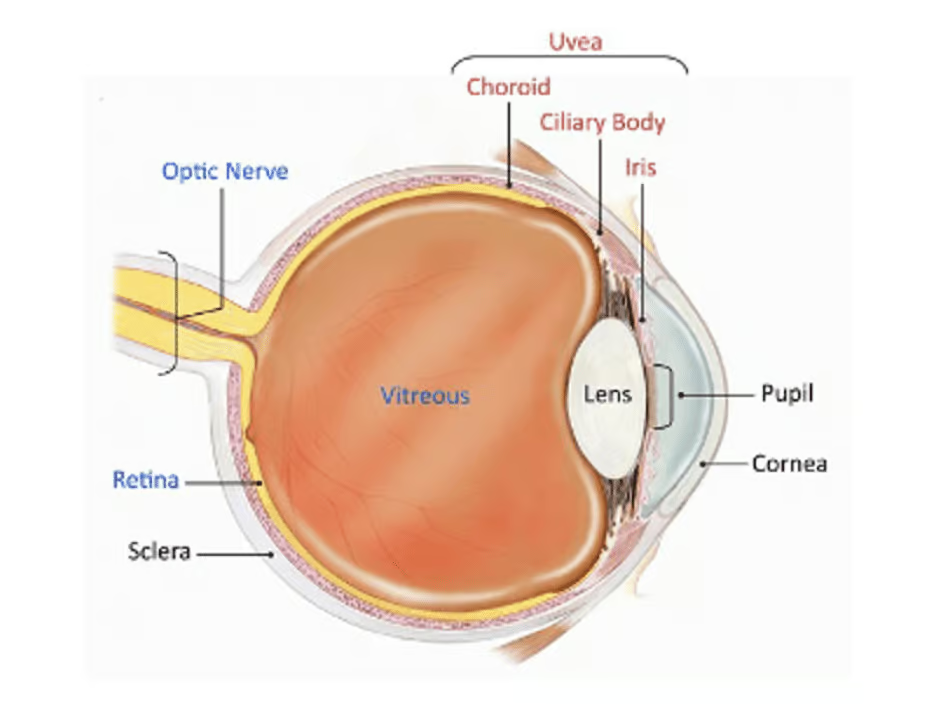
Uveitis presents as inflammation inside the part of your eye called the uvea and can also affect other parts of the eye. Uveitis can involve one or both eyes and can cause pain and redness in your eye(s), as well as vision loss. The condition sometimes resolves quickly, sometimes returns, and sometimes becomes chronic or long-term.
What Is The Uvea?
The uvea is the middle layer of the eye between the sclera (white part of the eye) and the retina (the light-sensitive layer at the back of the eye) and has three parts:
- Iris (colored part of the eye)
- Ciliary body (part of the eye that helps the lens focus)
- Choroid (part of the eye that connects the retina to the sclera)
What Are The Symptoms Of Uveitis?
Uveitis symptoms usually start suddenly and include:
- Blurry vision
- Floaters (small dark spots or squiggly lines that float across your vision)
- Eye pain
- Red eyes
- Sensitivity to light
See your eye doctor right away if you notice any of these symptoms because uveitis can cause vision loss if left untreated!
What Causes Uveitis?
The usual causes of uveitis are infection, injury, or an autoimmune or inflammatory disease; although, many times the cause is unidentified. If the cause is autoimmune, your body attacks healthy eye tissue. We do know that the condition more frequently affects individuals between 20 and 60 years old, cigarette smokers, and individuals with diseases that compromise the immune system.
Sometimes uveitis is caused by autoimmune diseases or immunodeficiency diseases such as:
- Ankylosing spondylitis
- Behcet’s disease
- Lupus
- Multiple sclerosis
- Psoriasis
- Rheumatoid arthritis
- Sarcoidosis
- Ulcerative colitis
- Vogt-Koyanagi-Harada (VKH) disease
- AIDS
How Can Your Eye Doctor Or Ophthalmologist Diagnose Uveitis?
Fortunately, diagnosing uveitis is simple and painless. Your ophthalmologist will perform a dilated eye exam to confirm a diagnosis of uveitis.
How Is Uveitis Treated?
Steroid medication is the usual first-line treatment for uveitis and can reduce inflammation in your eye, ease symptoms, and prevent vision loss. Most commonly, steroids are administered by prescription eye drops. However, other steroids may be used in the form of pills, injections near or in the eye, or eye implants that release steroids.
Steroids can have side effects and can increase your risk for cataracts and glaucoma. If you take steroids for uveitis, regular eye exams are important to monitor your progress and to check for signs of any problems. Your treatment plan will be determined by the affected part of your eye and any other health conditions. For example, your doctor may also prescribe some medications that control or quiet the immune response for longer-term prevention and management.
What Research Is Ongoing For Uveitis?
The National Eye Institute at the National Institutes of Health (a part of the United States government under the Department of Health and Human Services) conducts and funds many studies on uveitis including on causes and treatment. Cutting-edge research is being conducted through the Laboratory of Immunology.
Eye Health
We all now work (and play) on computers, many of us for long hours! To reduce eye strain, The Prevention of Blindness Society of Metropolitan Washington recommends children and adults take regular breaks using the 20-20-20 rule:
Every 20 minutes, shift your eyes away from the screen to look at an object at least 20 feet away for at least 20 seconds.
Everyone needs regular eye exams! The Bard was onto something important! Healthy eyes may reveal our soul, but they also are critical to a healthy body. Often, an eye condition is the initial warning to larger health issues. Take a minute to review The American Academy of Ophthalmology guidelines on eye screening: https://www.aao.org/eye-health/tips-prevention/eye-exams-101
About The Author
Dorothy Weinstein, M.A., has a long tenure working in health policy in Washington, D.C., and is a published author in health care delivery, biomedical research, technology, innovation, and environmental causes. She has been employed at Georgetown University: Institute of Health Policy Analysis, Association of American Medical Colleges, American Diabetes Association, The Endocrine Society, American College of Cardiology, and The National Health Council. Her expertise includes conducting large-scale research initiatives, developing advocacy programs, crafting legislation, lobbying on the local, state, and national levels, and directing government relations departments at leading nonprofit health organizations.
Sources
- Article Sources
González, M. M., Solano, M. M., Porco, T. C., Oldenburg, C. E., Acharya, N. R., Lin, S. C., & Chan, M. F. (2018). Epidemiology of uveitis in a US population-based study. Journal of ophthalmic inflammation and infection, 8(1), 6. https://doi.org/10.1186/s12348-018-0148-5
https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/uveitis