Untangling a Complex Web: How to Categorize Autoimmune Disease
The field of autoimmunity has greatly advanced over the last decades. We know more about the mechanisms behind immune system malfunctions, triggers of flare-ups, and ways to manage autoimmune disease signs and symptoms. Despite the continuous progress, autoimmune diseases are a heterogeneous and complex group of diseases that aren’t always easy to detect and categorize. Identifying an autoimmune disease is difficult because no single test can diagnose it. Also, many autoimmune diseases share similar signs and symptoms, which further complicates their identification. Therefore, the areas of diagnosis and classification need further research. Grouping autoimmune diseases according to well-defined criteria would help advance these areas and, in turn, guide disease monitoring and treatment to improve people’s health and quality of life.
Before discussing the challenges surrounding categorization, a few key terms should be defined. Also, sorting and categorizing autoimmune diseases can be difficult because of the overlap with other disease groups. The Autoimmune Registry defines an autoimmune condition either as a disease, syndrome, or comorbidity that develops when the immune system mistakes its own molecules and cells for harmful intruders (1). However, disease, syndrome, or comorbidity terms should not be used interchangeably (see table below). The existence of overlapping syndromes and disease subtypes complicates things further (see table below). Syndromes, comorbidities, overlapping syndromes, and subtypes aren’t always connected to autoimmunity and, thus, contribute to the overall challenge of assigning specific diseases to distinct categories.
Change from a state of health that causes harm to a person’s organ or system after the immune system attacks healthy cells
Collection of signs and symptoms that characterize an autoimmune disease
Presence of two or more autoimmune diseases in a person at the same time
OR
A distinct medical condition that co-occurs with an autoimmune disease (eg, endometriosis)
Presence of two or more autoimmune diseases or autoimmune symptoms for an extended period
A condition or complication of a disease that may appear in some people but not in others
How to Categorize Autoimmune Disease
Anatomical criteria
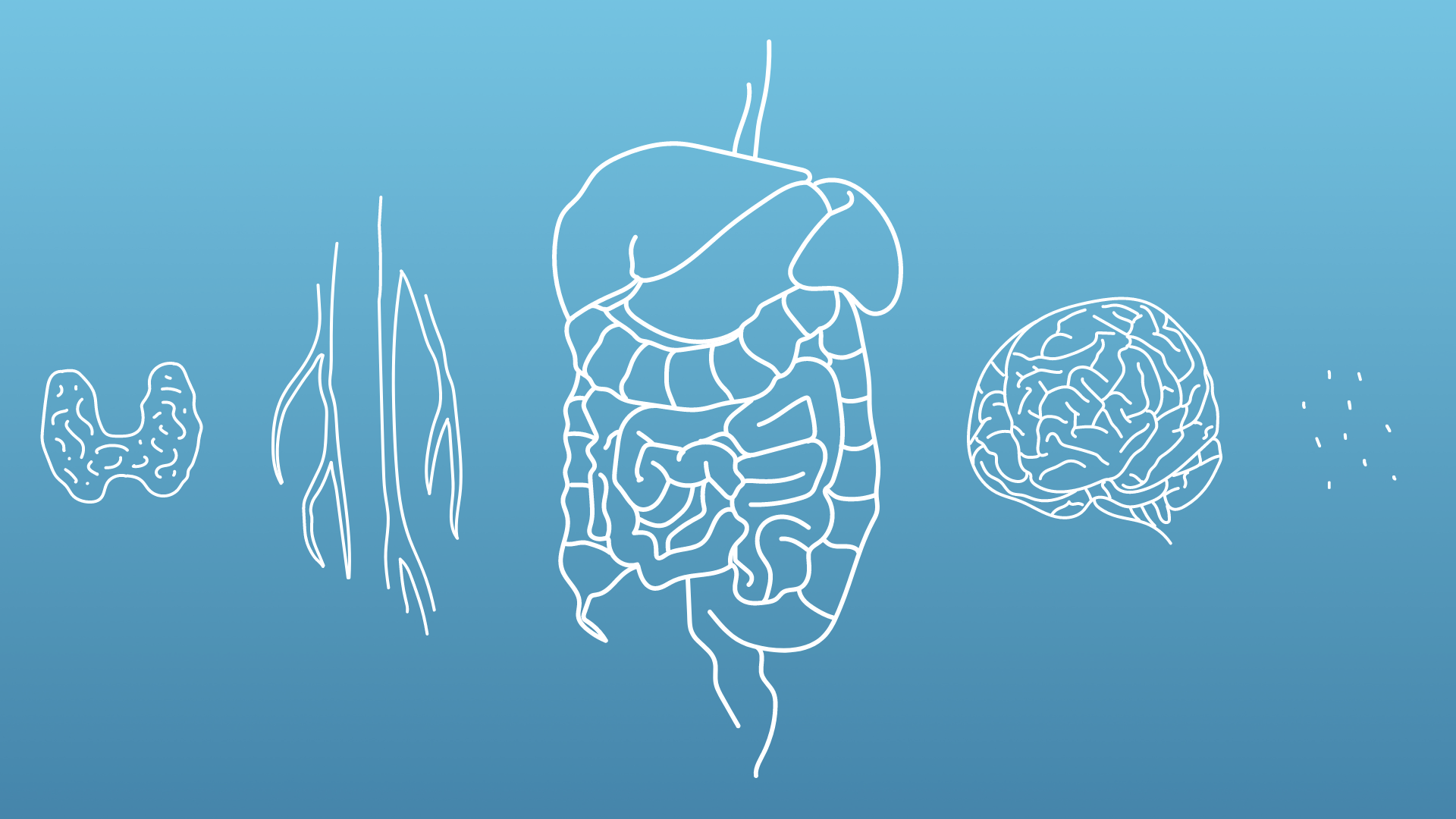
In clinical settings, autoimmune diseases are usually categorized depending on whether they affect either one or multiple organs.
In organ-specific autoimmune diseases, a person’s immune system attacks a single system, organ, or tissue. Examples include Graves’ disease in the thyroid gland, autoimmune hepatitis in the liver, and vitiligo in the skin. More autoimmune diseases grouped by organ or tissue are indicated in the figure below.
Systemic autoimmune diseases affect and damage multiple tissues and organs of the body and include systemic lupus erythematosus, rheumatoid arthritis, Sjogren’s syndrome, and dermatomyositis (1, 2, 3).
The classification of organ-specific and systemic autoimmune diseases can be supported by detecting and describing the histopathologic features of the affected tissues (3).
Immunologic criteria

Classification according to the location of the autoimmune attack is straightforward and clinically useful, but the drawback is that chronic inflammatory diseases may also be categorized as autoimmune even if they are not characterized by the B and T cells responses (adaptive immunity) typically observed in autoimmune diseases. Therefore, scientists and researchers have proposed categorizing autoimmune diseases according to their unique immunologic profiles (4, 5). For example, autoantibodies are invaluable markers for classifying, diagnosing, and identifying disease activity (5, 6). But one drawback is that autoantibodies’ connection to tissue damage tends to be more evident for organ-specific autoimmune diseases than for systemic autoimmune diseases (5). Analyzing aberrant (abnormal) T and B cells may be another approach to classification, which would involve closely looking at autoantigens and cellular immunity profiles (5).
Other approaches
Additional practices that help classifying and diagnosing autoimmune disease include laboratory and imaging techniques as well as proteomics, genomics, and metabolomic approaches that may assist in detecting autoantibodies, B and T cells, cytokines, organ-specific proteins, and molecular profiles (3, 7).
An alternative suggestion for categorizing autoimmune diseases may be to include them under the more heterogeneous group of “non-infectious inflammatory diseases”. This means they would be considered as part of a larger group of conditions that have self-directed inflammation in common but trigger different kinds of immune responses. Therefore, the type of diseases could be categorized according to their ability to stimulate either innate (autoinflammatory diseases) or adaptive immunity (autoimmune disease) (8, 9). This proposed classification method, however, would not solve the problem of using non-specific terms such as “inflammatory disease”, which may continue to cause overall confusion (5).
In a recent study, investigators used a process called “data mining” to sort through co-citations in the search engine, PubMed, and classify multiple autoimmune disease and comorbidities according to gender, age, prevalence, and body system (10). Processes that allow scientists to analyze complex databases hold promise in categorizing this complex group of diseases and other associated conditions, but additional research is needed to explain why certain conditions are observed more in some groups than others (10).
Finding new and improved classification methods will guide disease diagnosis and monitoring, helping health care workers to better treat patients with an autoimmune disease.

About The Author
Sources
- Article Sources
Autoimmune Registry. Autoimmune condition classification. https://www.autoimmuneregistry.org/disease-classification
Johns Hopkins Medicine. Classification of Autoimmune Diseases. https://pathology.jhu.edu/autoimmune/classification/
Wang L et al. (2015). Human autoimmune diseases: a comprehensive update. Journal of Internal Medicine, 278(4):369-95. https://pubmed.ncbi.nlm.nih.gov/26212387/
Davidson A. & Diamond B. (2001). Autoimmune disease. New England Journal of Medicine, 345(5):340-50. https://pubmed.ncbi.nlm.nih.gov/11484692/
Pisetsky D.S. (2023). Pathogenesis of autoimmune disease. Nature Reviews Nephrology, 19(8):509-524. https://pubmed.ncbi.nlm.nih.gov/37165096/
Sciascia S. et al. (2023). Autoantibodies testing in autoimmunity: Diagnostic, prognostic and classification value. Autoimmunity Reviews, 22(7):103356. https://pubmed.ncbi.nlm.nih.gov/37150488/
Maecker H.T. et al. (2012). New tools for classification and monitoring of autoimmune diseases. Nature Reviews Nephrology, 8(6):317-28. https://pubmed.ncbi.nlm.nih.gov/22647780/
Grateau G. et al (2013). How should we approach classification of autoimmune diseases? Nature Reviews Nephrology, 9(10):624-9. https://pubmed.ncbi.nlm.nih.gov/23838615/
McGonagle D. & McDermott M.F (2005). A proposed classification of the immunological diseases. PloS Medicine, 3(8):e297. https://pubmed.ncbi.nlm.nih.gov/16942393/
Samuels H. et al. (2022). Autoimmune Disease Classification Based on PubMed Text Mining. Journal of Clinical Medicine, 11(15):4345. https://pubmed.ncbi.nlm.nih.gov/35893435/