Personalized Medicine for Autoimmune Diseases

If you have an autoimmune disease, chances are you might have to try several treatments before finding one that works. That could mean several months of unsuccessful treatments before landing on one that works.
“The current challenges in autoimmune disease treatment is that not all patients respond to the current available treatments,” says Dr. Georg Schett, Vice President Research at Friedrich-Alexander University of Erlangen-Nuremberg. “There is a fraction of patients who do not achieve remission of disease and they are at risk for developing organ damage.”
With advances in genomics and other molecular tests that are paving the way for personalized medicine, it’s becoming possible to avoid scenarios such as this.
What is Personalized Medicine?
As the name suggests, personalized medicine tailors therapies to each individual patient. This is often done based on a person’s genetic profile, lifestyle, and environment. In contrast to a “one-size-fits-all” approach, personalized medicines could help improve drug effectiveness while reducing side effects. It is also known as precision medicine.
Examples of personalized medicine include:
- Using a person’s genetic profile to identify best treatment:
- Using cytokine profiles to determine biologic drug choice
- Identifying disease-specific autoantibodies to guide therapies
- CAR-T cell therapy that modifies a person’s own T cells to target and deplete B cells involved in autoimmunity
Currently, personalized medicine is used in treating cancer, where a person’s tumor is removed and sequenced to identify the mutations that the patient has. Based on these mutations, doctors can determine the best treatments for individuals with those particular mutations (1). Building upon this work, personalized medicine has the potential to make tremendous impacts in treating autoimmunity.
Why Personalized Medicine Matters in Autoimmune Disease
One of the reasons that autoimmune diseases are well-suited for personalized medicine is because “autoimmune diseases can be very heterogeneous,” says J. Michelle Kahlenberg, Professor of Rheumatology at the University of Michigan. “Patients can have different types of manifestations, and they can also have different reasons for having those manifestations based on their genetics and exposures.”
While heterogeneity exists in many autoimmune diseases, a great example of heterogeneity is lupus, which can affect different organs and present with different symptoms in different people (2). “It’s really the poster child for heterogeneity,” says Kahlenberg. “It’s been hard to find treatments that are blockbusters for lupus.”
Due to this heterogeneity, it becomes challenging to identify the most effective treatment. Currently, treatment is a trial-and-error approach dictated by insurance guidelines, often based on cost. Personalized medicine “gives us evidence to take to the insurance company and say, ‘you really need to cover this treatment because this is what’s driving this person’s disease’ as opposed to them using a blanket approach, which is ‘you have to try X, Y, and Z on everybody before we’ll even think about any of these other types of therapies,’” Kahlenberg explains.
Understanding Disease Subtypes and Biomarkers
Before personalized medicine approaches can make it into the clinic for treatments, scientists must first understand the different subtypes within a specific disease using data from genome and RNA sequencing, blood samples, and/or biopsies from affected sites (3, 4, 5). Kahlenberg heads such a project at the University of Michigan to study autoimmune skin diseases . The goal of this project is identify biological underpinnings behind the symptoms patients are experiencing so that this information can be used to develop and implement more targeted therapies tailored to individuals.
Research such as these can help researchers develop point-of-care testing that could enable quick diagnosis and inform treatment options. Kahlenberg gives an example: If we knew a particular cell type was critical for a response to Drug X and we had a way to quickly test for that cell type, we could implement therapy faster without trying other drugs and failing them.
Personalized CAR T-Cell Therapy: A New Frontier
Another form of personalized medicine is CAR T-cell therapy. “Disease [resistant to conventional treatment] or severe disease with organ involvement is a critical indication point for CAR T-cell therapy,” Schett says.
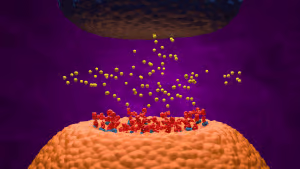
While CAR-T is known for its use in treating cancer, Schett has been a pioneer of this approach for treating autoimmune diseases (6). This approach uses T cells extracted from the patient’s blood and modifies them to target antigens of interest (ex: surface proteins on B cells, including autoreactive B cells). After infusing these cells into the patient, B cells are eliminated and after about 100 days, the B cell population comes back without the autoimmune-associated B cells (7).
The beauty of CAR T-cell therapy is that it contrasts with the majority of autoimmune disease treatments that aren’t curative and require patients to stay on the therapies indefinitely. “The big challenge in the future is really how to do curative approaches, which allows the patients to stop immunosuppressive drugs,” says Schett. CAR T-cell therapy has potential to solve this challenge. “It’s a single infusion stopping the disease, and you don’t need additional immunosuppressive treatment for a long time,” he adds. His current studies have found that remission lasts at least four years, but it’s possible that remission can be lifelong. “For the patient, this is a huge step forward.”
While this approach is very individualized and can be very expensive and intensive to prepare, Schett is hopeful about the possibility of an off-the-shelf CAR T-cell therapy using T cells from donors. It can be more scalable and cost effective, he says. Because these types of therapies are so new, it’s unclear whether they can achieve sustained drug-free remission that has been seen from CAR T-cell therapy using the patient’s own T cells.
The Future of Personalized Medicine in Autoimmune Care
With advances in sequencing, cell profiling, AI, and CAR T-cell therapy, personalized medicine is advancing at a fast pace. One day in the future, we may be able to better predict how a person will respond to specific treatments so that we can deliver more effective treatments more quickly to patients.
“Research is important. It has to be a priority to invest in these things if this is what patients want to be available 10 years from now,” says Kahlenberg. “If we don’t have the funding to do [this type of work], we’re going to be in the same situation where we are now where we’re using a lot of steroids to bridge people when we don’t have better therapies to give them.”

About the Author
Sources
- Article Sources
Addala, V., Newell, F., Pearson, J. V., Redwood, A., Robinson, B. W., Creaney, J., & Waddell, N. (2024). Computational immunogenomic approaches to predict response to cancer immunotherapies. Nature reviews. Clinical oncology, 21(1), 28–46. https://doi.org/10.1038/s41571-023-00830-6
Owen, K. A., Grammer, A. C., & Lipsky, P. E. (2022). Deconvoluting the heterogeneity of SLE: The contribution of ancestry. The Journal of allergy and clinical immunology, 149(1), 12–23. https://doi.org/10.1016/j.jaci.2021.11.005
Berthier, C. C., Tsoi, L. C., Reed, T. J., Stannard, J. N., Myers, E. M., Namas, R., Xing, X., Lazar, S., Lowe, L., Kretzler, M., Gudjonsson, J. E., & Kahlenberg, J. M. (2019). Molecular Profiling of Cutaneous Lupus Lesions Identifies Subgroups Distinct from Clinical Phenotypes. Journal of clinical medicine, 8(8), 1244. https://doi.org/10.3390/jcm8081244
Tsoi, L. C., Gharaee-Kermani, M., Berthier, C. C., Nault, T., Hile, G. A., Estadt, S. N., Patrick, M. T., Wasikowski, R., Billi, A. C., Lowe, L., Reed, T. J., Gudjonsson, J. E., & Kahlenberg, J. M. (2020). IL18-containing 5-gene signature distinguishes histologically identical dermatomyositis and lupus erythematosus skin lesions. JCI insight, 5(16), e139558. https://doi.org/10.1172/jci.insight.139558
Abernathy-Close, L., Lazar, S., Stannard, J., Tsoi, L. C., Eddy, S., Rizvi, S. M., Yee, C. M., Myers, E. M., Namas, R., Lowe, L., Reed, T. J., Wen, F., Gudjonsson, J. E., Kahlenberg, J. M., & Berthier, C. C. (2021). B Cell Signatures Distinguish Cutaneous Lupus Erythematosus Subtypes and the Presence of Systemic Disease Activity. Frontiers in immunology, 12, 775353. https://doi.org/10.3389/fimmu.2021.775353
Müller, F., Taubmann, J., Bucci, L., Wilhelm, A., Bergmann, C., Völkl, S., Aigner, M., Rothe, T., Minopoulou, I., Tur, C., Knitza, J., Kharboutli, S., Kretschmann, S., Vasova, I., Spoerl, S., Reimann, H., Munoz, L., Gerlach, R. G., Schäfer, S., Grieshaber-Bouyer, R., … Schett, G. (2024). CD19 CAR T-Cell Therapy in Autoimmune Disease – A Case Series with Follow-up. The New England journal of medicine, 390(8), 687–700. https://doi.org/10.1056/NEJMoa2308917
Schett G, Nagy G, Krönke G, Mielenz, D. (2024). B-cell depletion in autoimmune diseases. Annals of the Rheumatic Diseases 83:1409-1420. https://doi.org/10.1136/ard-2024-225727