Infection and Immunity: Turning the Lens on Microbes
Infections can influence the development and progression of autoimmune diseases. In order to understand the intricate relationship between infections and autoimmune diseases, it is crucial to take microbial influence on autoimmunity into perspective.
Infection – the invasion of a body system or organ by microbes – has been known as a key player in autoimmune disease development. Most autoimmune diseases or flare-ups have been associated with at least one infection, and a single infection can trigger multiple autoimmune diseases or flare-ups. People with an autoimmune disease are also at higher risk of infection, even while receiving treatment for that disease (1).
Infection activates multiple components of the immune system, leading to immune dysregulation – a set of abnormal changes that disrupt the immune system (2). Although immune dysregulation may be induced without infection, microbes initiate autoimmunity in many susceptible people (2, 3). Infection can also trigger signs, symptoms, and flare-ups and move more quickly in those who already have an autoimmune disease.
Understanding Infection’s Influence on Autoimmunity
Infection induces autoimmunity by activating autoantibodies and cells through different mechanisms. The following terms are helpful to know:
Antibodies that recognize antigens inherently present in the body of patients who have an autoimmune disease. These antigens are called autoantigens or self-antigens.
Persistent infection constantly stimulates the immune system and, thus, releases self-peptides, causing the tissue damage typical of autoimmune disease.
Infection triggers a “cascade” of immune events in people with immune diseases like multiple sclerosis, leading to inflammation and swelling in different organs.
These microbial parts potently activate large numbers of T cells, which can dramatically change the immune system. These factors have been associated with the signs, symptoms, and flare-ups of psoriasis.
When the processes that recognize and fight microbes (e.g., phagocytosis) are deeply altered, the immune system cannot effectively fight off infection. This commonly occurs in people with lupus.
This cascade-like process helps antibodies and immune cells attack and clear microbes from the body. Excessive activation and defects of the complement system may lead to the development of disorders like lupus and vasculitis (4).
Turning The Lens On Bacteria, Parasites, And Fungi
Microbial infections influence the course of autoimmune disease in combination with other factors, such as the inner characteristics of a population or an individual person (1, 5).
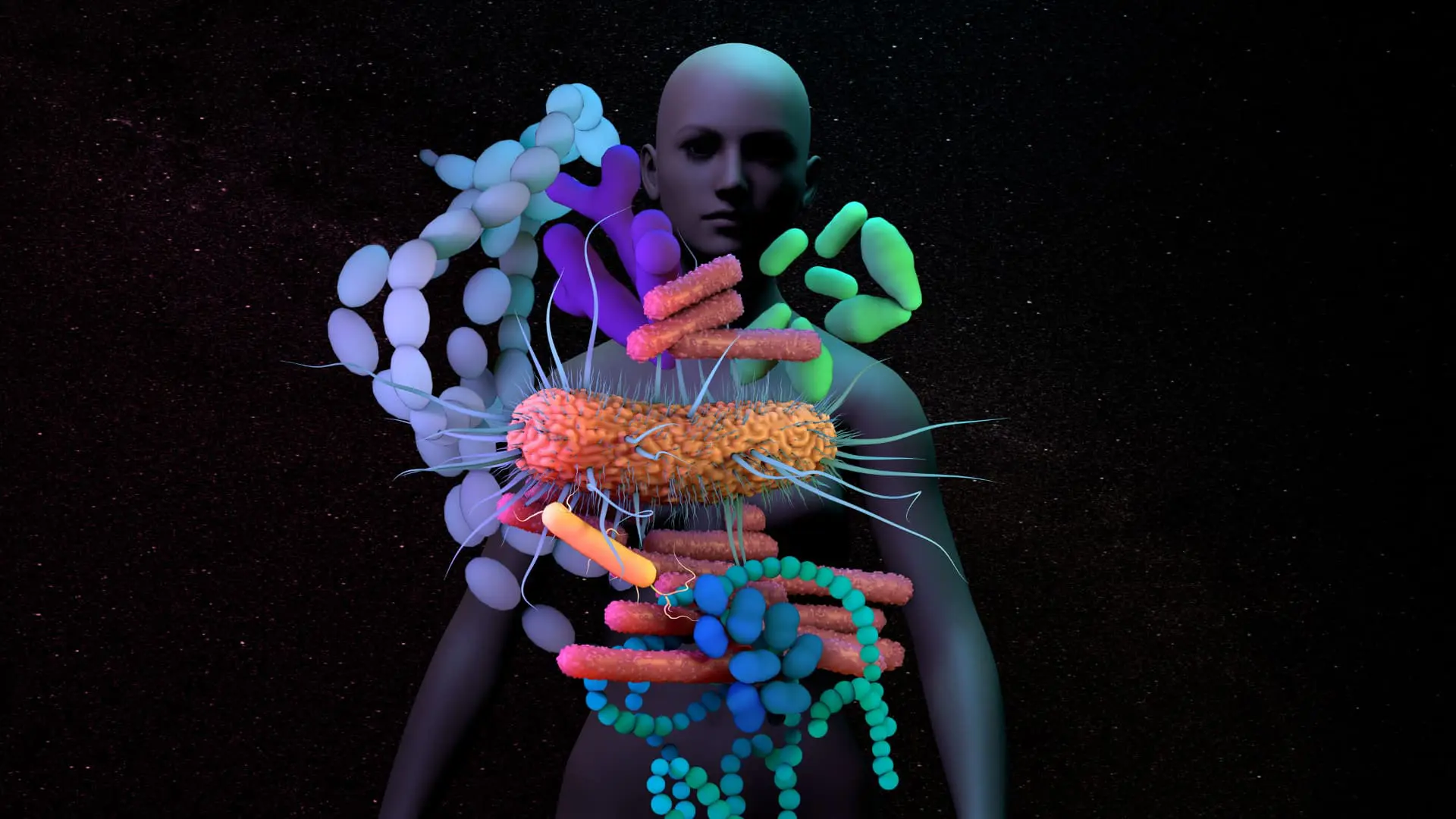
A person’s microbiota consists of microbial communities that live in different body systems. Non-pathogenic (harmless) microorganisms like bacteria, protozoa, and fungi often cohabit in harmony in different body organs and promote human health in multiple ways. However, changes and imbalances in these microbial communities can turn “peaceful” microorganisms into opportunistic microbes, turning them into pathogens (capable of causing disease).
Microbes that trigger autoimmunity are not always part of the body’s microbiota but can access organs and systems from the outside. Fundamentally, they invade the body and activate disease as foreign agents.
Although investigators have studied the relationship between viruses and autoimmune disorders like lupus, Sjögren’s syndrome, celiac disease, and multiple sclerosis (6), the focus here will be on bacteria, parasites, and fungi.
Research studies using genetic tools such as infectomics (the study of structural and functional genomics and proteomics of microbial infections) and autoinfectomics (the study of infectious-induced autoimmunity) will help us understand the relationship between these microbes and autoimmunity and explain why some people are more susceptible and why others may develop more than one autoimmune disease (7).
Bacteria
Infections caused by bacteria may trigger immune responses that either initiate or aggravate autoimmune diseases (3). For example, gastroenteritis caused by Salmonella and genital infections caused by Chlamydia may trigger reactive arthritis, which affects the joints and eyes and can last for several years (3).
Signs and symptoms of autoimmune arthritis may also be observed in people with untreated Lyme disease, tuberculosis, and urinary tract infections (1, 3, 8, 9).
The stomach pathogen Helicobacter pylori, the enteric pathogen Escherichia coli, and the respiratory pathogen Streptococcus pneumoniae have all been associated with lupus (1, 10). Streptococci may also be involved in psoriasis development.
Acinetobacter and Pseudomonas aeruginosa, were found to trigger autoantibodies against a myelin-specific protein and, thus, may play a role in multiple sclerosis development (1).
Some bacteria form thin layers that stick to body surfaces, known as biofilms, which increase a microbe’s ability to cause disease. Biofilms carry structures that resemble the host’s, activating autoimmune responses (3).
Parasites
Research studies have suggested that chronic infections caused by parasites like protozoa and worms may be linked to autoimmunity (2).
Examples of protozoa (microbial parasites made of one cell) include Plasmodium, which causes malaria, and Leishmania, responsible for leishmaniasis. Autoantibodies and autoimmune anemia have been detected in patients with malaria, but the connection with autoimmunity is poorly understood (11). Cases of visceral leishmaniasis were associated with lupus, autoimmune hepatitis, and primary biliary cirrhosis (2).
The production of autoantibodies has also been observed with parasitic worm infections caused by fluke flatworms and roundworms (2). Parasitic worms are also being studied for use in autoimmunity therapy, but their role in autoimmune disease and health is still unclear (12, 13).
Fungi
Exposure to molds (fungi) and the toxins they produce (mycotoxins) is known to influence human microbiota and immunity and lead to the development of different diseases. Molds are known to trigger respiratory conditions such as asthma, and mycotoxins may have long-term effects such as cancer (14, 15).
Although the involvement of molds and mycotoxins is well established in allergy, their role in autoimmunity is still being investigated. They were found to be linked to multiple sclerosis and rheumatoid arthritis in people with pre-existing immune dysregulation (14, 16).
Evidence of the Candida yeast (also a fungus) was found in patients with multiple sclerosis, but the mechanisms behind this relationship are not fully understood (17, 18).
Minimizing The Risks Of Infection
If you have an autoimmune disease, take action to minimize the risks of infection.
Practice good hand hygiene and avoid contact with people who are sick. Regularly check food for signs of mold and buy dry items such as rice and nuts as often as possible. Store and refrigerate food properly to eliminate the risk of both bacterial and fungal contamination.
Always talk to your doctor about your concerns before taking any additional steps.
About The Author
Damiana Chiavolini, MS, PhD is a freelance writer who specializes in medical and life science topics. As a trained researcher, she authored journal articles in the areas of infection and immunity and wrote booklets and book chapters about different diseases. As a professional communicator, she writes feature articles for magazines and other publications and produces content for higher education platforms. Damiana is also an experienced academic editor, microbiology educator, writing coach, and fragrance blogger. She is a contributing member of the American Medical Writers Association and the immediate past-president of the association’s Southwest Chapter.
Sources
- Article Sources
Arango M.T., Schoenfeld Y., Cervera R., & Anaya J.M. (2013). Infection and Autoimmune Disease. Autoimmunity: From Bench to Bedside. El Rosario University Press.https://www.ncbi.nlm.nih.gov/books/NBK459437/
Abu-Shakra (2015). Parasitic Infection and Autoimmunity. Infection and Autoimmunity (Second Edition).https://www.sciencedirect.com/science/article/abs/pii/B9780444632692000404
Nicastro L. & Tükel Ç. (2019). Bacterial amyloids: The link between bacterial infections and autoimmunity. Trends in Microbiology, 27(11), 945-963. https://pubmed.ncbi.nlm.nih.gov/31422877/
Conigliaro P., Triggianese P., Ballanti E., Perricone C., Perricone R., & Chimenti M.S. (2019). Complement, infection, and immunity. Current Opinions in Rheumatology, 31(5), 532-541.https://pubmed.ncbi.nlm.nih.gov/31192812/
Ercolini A.M. & Miller S.D (2009). The role of infections in autoimmune disease. Clinical Experimental Immunology, 155(1), 1-15. https://pubmed.ncbi.nlm.nih.gov/19076824/
Smatti M.K., Cyprian F.S, Nasrallah G.K., Asmaa A.A.T., Almishal R.O., & Yassine H.M. (2019). Viruses and Autoimmunity: A Review on the Potential Interaction and Molecular Mechanisms. Viruses, 11(8), 762.https://pubmed.ncbi.nlm.nih.gov/31430946/
Bogdanos DP, Smyk D.S., Rigopolou E.I., Sakkas L.I., & Schoenfeld Y. (2015). Infectomics and autoinfectomics: a tool to study infectious-induced autoimmunity. Lupus, 24(4-5), 364-73.https://pubmed.ncbi.nlm.nih.gov/25801879/
Lochhead R.B., Strle K., Arvikar S.L., Weis JJ., & Steere A.C (2019). Lyme arthritis: linking infection, inflammation and autoimmunity. Nature Reviews Rheumatology, (8), 449-461.https://pubmed.ncbi.nlm.nih.gov/34226730/
Starshinova A., Malkova A., Kudryavtsev I., Kudlay D., Zinchenko Y., & Yablonskiy P. (2022). Tuberculosis and autoimmunity: Common features. Tuberculosis, 134, 102202. https://pubmed.ncbi.nlm.nih.gov/35430551/
Qiu C.C., Caricchio R., & Gallucci S (2019). Triggers of Autoimmunity: The Role of Bacterial Infections in the Extracellular Exposure of Lupus Nuclear Autoantigens. Frontiers in Immunology, 10, 2608.https://pubmed.ncbi.nlm.nih.gov/31781110/
Rivera-Correa J. & Rodriguez A. (2020). Autoimmune Anemia in Malaria. Trends in Parasitology, 36(2), 91-97. https://pubmed.ncbi.nlm.nih.gov/31864893/
Krawczak K., Donskow-Łysoniewska K., & Doligalska M (2017). Regulatory function of parasites in autoimmune disease – outcome from experimental model infection. Annals of Parasitology, 63(1), 7-14.https://pubmed.ncbi.nlm.nih.gov/28432858/
Zaccone P., Fehervari Z., Phillips J.M., Dunne D.W., & Cooke A. (2006). Parasitic worms and inflammatory disease. Parasite Immunology, 28(10), 515-23. https://pubmed.ncbi.nlm.nih.gov/16965287/
Kraft S., Buchenauer L., & Polte T. (2021). Mold, Mycotoxins and a Dysregulated Immune System: A Combination of Concern? International Journal of Molecular Sciences, 22(22), 12269.https://pubmed.ncbi.nlm.nih.gov/34830149/
World Health Organization. Mycotoxins. https://www.who.int/news-room/fact-sheets/detail/mycotoxins
Purzycki C.B. & Shain D.H. (2010). Fungal toxins and multiple sclerosis: a compelling connection. Brain Research Bulletin, 29(9):1139-45. https://pubmed.ncbi.nlm.nih.gov/20214953/
Benito-León J., Pisa D., Alonso R., Calleja P., Díaz-Sánchez M., & Carrasco L. (2010). Association between multiple sclerosis and Candida species: evidence from a case-control study. European Journal of Clinical Microbiology & Infectious Diseases, 29(9):1139-45. https://pubmed.ncbi.nlm.nih.gov/20556470/
Pisa D., Alonso R., Jimenez-Jimenez F.J., & Carrasco L. (2013). Fungal infection in cerebrospinal fluid from some patients with multiple sclerosis. European Journal of Clinical Microbiology & Infectious Diseases, 32(6):795-801. https://pubmed.ncbi.nlm.nih.gov/23322279/











