Is Long Covid a New Autoimmune Disease?

A pathologist weighs in on the latest research involving the link between autoimmunity and Long Covid
The more we learn about Long COVID—one of the terms for the health problems that appear or worsen in some people weeks to months after acute SARS-CoV-2 infection—the more confusing the picture becomes. The disease can cause a dizzying array of more than 200 possible symptoms and can follow even mild or asymptomatic infections (1,2). Presently, there are no standard therapies or medications to treat Long COVID symptoms.

Model of the SARS-CoV-2 virus. Photo: NIH
One of the most troubling mysteries about Long COVID, also known as long-haul COVID or post-COVID syndrome, is what occurs in the bodies of patients to drive this persistent and often distressing condition. One theory is that Long COVID could be an autoimmune disease (AD). To illustrate this possibility, studies have noted shared symptoms between Long COVID and suspected ADs like chronic fatigue syndrome (ME/CFS) and fibromyalgia- including persistent fatigue, widespread muscle pain, memory difficulties, and mood disorders (3,4).
If the autoimmune theory pans out-and that is still a big if– SARS-CoV-2 would join a long list of viruses that are strongly implicated in the development of AD based on the fact that the infection coincides with disease onset and the appearance of autoantibodies, autoreactive T cells, and other features of autoimmune disease. Other probable viral triggers of chronic illness include Epstein-Barr virus (EBV), which is thought to be a trigger for lupus in certain individuals, and influenza, which has been linked to the development of type 1 diabetes (5,6).
“It is certainly possible that SARS-CoV-2 infection could induce autoimmune problems”
says Dr. Eline Luning Prak, a professor of pathology and laboratory medicine at the Hospital of the University of Pennsylvania. But the path to being able to categorize Long COVID as a bona fide AD is a long one. “We will probably never know that completely—and there will probably be different ways of generating something that is long COVID,” with autoimmunity being involved in only some patients, Luning Prak says.

SARS-CoV-2 infection. Photo: NIH
Much of the research exploring the autoimmune properties of Long COVID has revolved around autoantibodies, which have been detected in a large proportion (about half in some studies) of patients who are severely ill with acute COVID-19 (7). A hallmark of many autoimmune diseases, autoantibodies wreak havoc by recognizing and interfering with the body’s own proteins, DNA, and other molecules, known altogether as self-antigens.
Studies have now documented a laundry list of different autoantibodies that are present during acute COVID-19 infection. One study found autoantibodies against ACE2 among a small group of patients hospitalized with COVID, as well as a group that had recovered from infection. ACE2, which the SARS-CoV-2 virus uses to gain entry into cells, is an important player in controlling inflammation (8). Autoantibodies that inhibit ACE2 may contribute to persistent inflammation, which is a central feature of many ADs and is thought to be involved in Long COVID.
Evidence of a link between autoantibodies and Long COVID symptoms is also building. Among the most incriminating are autoantibodies that bind to cell surface proteins called G-protein coupled receptors (GPCRs) and may block the messages these proteins convey to cells to control immune and other functions. Various GPCR antibodies are thought to contribute to ADs including ME/CFS, rheumatoid arthritis, and Sjogren’s syndrome. Last spring, a small study of individuals experiencing Long COVID symptoms—particularly neurological (fatigue, etc) and cardiovascular (elevated heart rate, etc)—found that all had GPCR autoantibodies (9).
Making the case for autoantibodies
In order to definitively link Long COVID to autoantibody activity, several criteria still need to be met, Dr. Luning Prak says. For one, “it would be really nice to know if patients had the autoantibodies all along or if the virus-induced them,” she notes. If SARS-CoV-2 infection does indeed spur the production of new autoantibodies, it could happen through several possible mechanisms. For example, the infection may provoke such a strong immune response—an “all hands on deck” response, as Dr. Luning Prak describes —that the immune system begins to turn on itself. Another possible factor is molecular mimicry, in which components of the virus resemble human proteins, causing the immune system to mistakenly attack the body’s own healthy tissues and organs.
A recent study by Dr. Luning Prak and her colleagues found that, in a small group of patients hospitalized with COVID-19, autoantibody levels rose as infection progressed. These findings suggest that SARS-CoV-2 could stimulate autoantibody production. Additionally, a Yale study reported that autoantibody production began ramping up at the same time as antiviral antibodies (10).
It is also possible that SARS-CoV-2 infection unearths a pre-existing autoimmune disease or predisposition in some patients. A recent study of patients hospitalized with COVID-19 found that some had autoantibodies prior to infection, including types that have been associated with lupus (11).
Another question that should be fleshed out, Dr. Luning Prak notes, is whether autoantibodies that are present around the time of acute infection persist in patients with Long COVID.
In 2021, a small study of Long COVID patients found that 44% had high levels of antinuclear antibodies (ANAs), a group of autoantibodies associated with lupus and other autoimmune diseases. These autoantibodies remained present for as long as 12 months after SARS-CoV-2 infection (12). The group was also more likely to have neurocognitive problems, such as difficulty concentrating, than those with low ANA levels.
Even though Dr. Luning Prak’s team found a diverse array of autoantibodies among patients in their study, each patient produced autoantibodies that target only a small number of self-antigens during acute infection. As such, it seems that COVID-19 could randomly trigger a loss of immune tolerance to a small set of self-antigens that results in the immune system attacking specific tissues and organs, just like in many ADs. If it can be demonstrated that certain autoantibodies are associated with specific symptoms of long COVID, “that would help strengthen the case” that there is an underlying autoimmune cause, Dr. Luning Prak says. In the context of acute COVID-19, there is evidence of autoantibodies targeting a range of self-antigens in the lungs, central nervous system, and other organs that have been implicated in Long COVID disease.
Broadening the search for immune drivers
Many autoimmune diseases are the result of a complex interplay of immune responses that involve the production of destructive autoantibodies, as well as autoreactive T-cells, which recognize self molecules called peptides— and innate immune cells, which are thought to harbor sensing molecules that can turn on self-antigens.
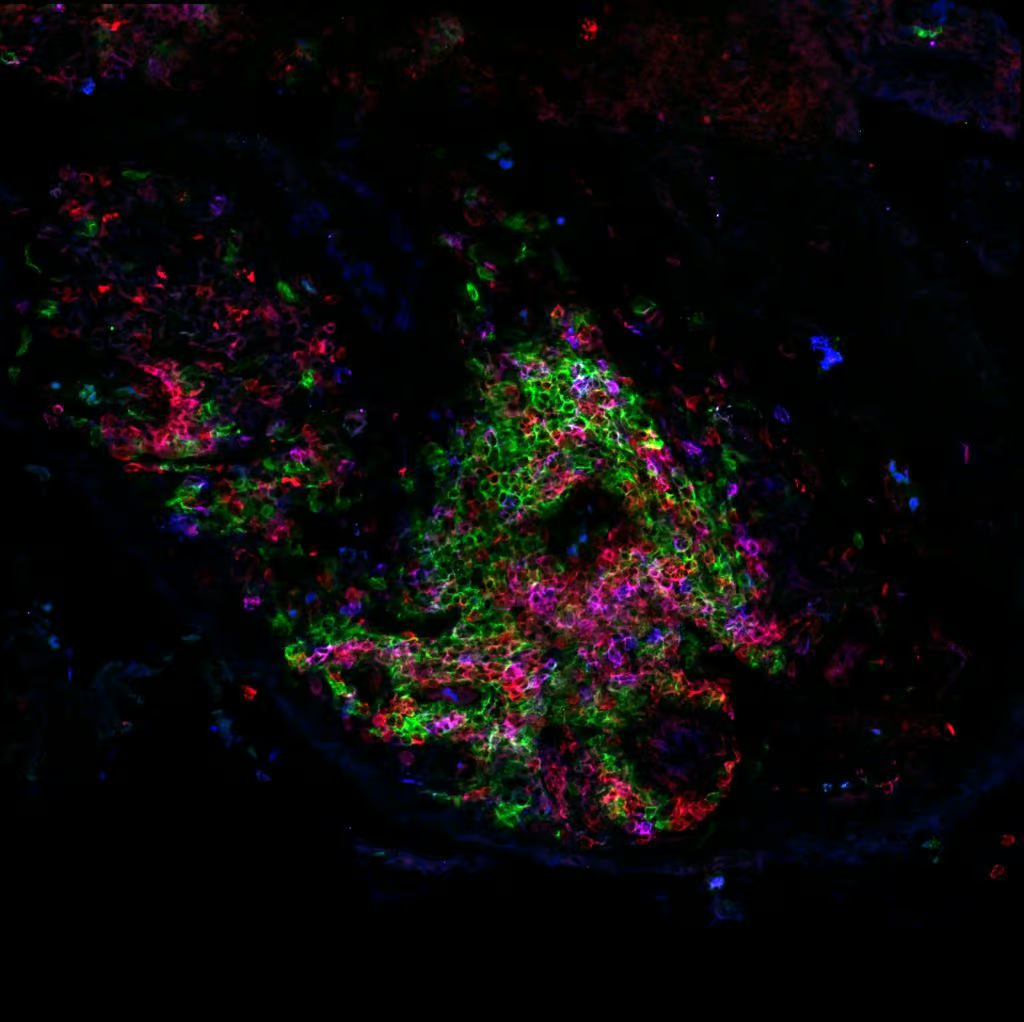
T- and B- cells, like the ones pictured here, are involved in the production of harmful autoantibodies in patients with autoimmune disease. Photo: NIH
Although measuring T-cell and innate immune responses is more technically challenging than detecting autoantibodies, emerging research aims to understand their role in acute COVID-19 infection and Long COVID. Over the last year, researchers at the Institute for Systems Biology in Seattle, Washington endeavored to profile the immune systems of Long COVID patients 2 to 3 months following acute infections ranging from mild to severe. In the small study, researchers found an expanded population of cytotoxic T-cells at 2 to 3 months compared with the acute phase of infection, specifically in a small subset of patients (9%) who were experiencing gastrointestinal symptoms (11). Cytotoxic T-cells are increasingly recognized as playing a role in autoimmune diseases (13).
A recent study by researchers in Australia followed people for 8 months after mild or moderate SARS-CoV-2 infection and found evidence for widespread “immunological dysfunction”—disruptions in B and T-cell and innate immune responses—among individuals who continued to have Long COVID symptoms (14). Compared with a small group of people who had recovered from infection, those experiencing Long COVID had higher levels of a set of immune-signaling molecules that altogether suggested ongoing inflammation. The study also found ongoing activation of cytotoxic T cells and certain classes of innate immune cells.
Parsing the possibilities
Despite the growing evidence that Long COVID may be a type of autoimmune disease—and some experts are already calling it an “autoimmune-related disorder”— a case can be made for other causes. Leading the pack of alternative explanations is that proteins or RNA from the SARS-CoV-2 virus may remain in tissue, or the virus itself may actually continue to replicate in some individuals, driving chronic inflammation. In support of this theory is the fact that viral proteins and/or RNA have been found in a range of tissue types, including respiratory, cardiac, renal, brain, and muscle, months after COVID-19 infection (16).
Another potential cause of Long COVID is that the body could be responding to unresolved tissue damage. This explanation is more feasible for people who had severe infections, particularly those who were in the ICU and likely lost muscle mass.
Unearthing the causes of Long COVID is far more than an academic exercise because it could pave the way for developing treatments. Last year, doctors gave a 59-year-old man an experimental drug for his glaucoma that blocks GPCR autoantibodies (17). The patient also suffered from Long COVID and had autoantibodies against GPCRs. In addition to improvements in his glaucoma, the man recovered from fatigue, brain fog, and loss of taste for at least four weeks. Experts hope that breakthroughs like these will give way to improvements in research, diagnosis, and treatment for Long COVID.
“There are a lot of nice therapies that we can use to target people’s B-cells [if a subset of people with Long COVID can be shown to have B-cell disorders],” Dr. Luning Prak says. “Maybe that can put them into remission from Long COVID and maybe they never have it again.”
Sources
- Article Sources
Davis HE. et al. 2021. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 38:101019.
Bliddal S. et al. 2021. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci Rep 11:13153
Wostyn P. 2021. COVID-19 and chronic fatigue syndrome: Is the worst yet to come? Med Hypotheses 146: 110469
Dotan A. et al. 2022. The autonomic aspects of the post-COVID19 syndrome. Autoimmun Rev 21: 103071
Knight JS. et al. 2021. The intersection of COVID-19 and autoimmunity. J Clin Invest 131:e154886
Smatti MK. et al. 2019. Viruses and Autoimmunity: A Review on the Potential Interaction and Molecular Mechanisms. Viruses 11:762
Chang SE. et al. 2021. New-onset IgG autoantibodies in hospitalized patients with COVID-19. Nat Commun 12, 5417
Arthur JM. et al. 2021. Development of ACE2 autoantibodies after SARS-CoV-2 infection. PLoS ONE 16: e0257016
Wallukat G. et al. 2021. Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J Transl Autoimmun 4:100100.
Wang EY. et al. 2021. Diverse functional autoantibodies in patients with COVID-19. Nature 595, 283–288
Su Y. et al. 2022. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185:881-895
Seeßle J. et al. 2022. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin Infect Dis 74:1191-1198
Deng Q. et al. 2019. The Emerging Epigenetic Role of CD8+T Cells in Autoimmune Diseases: A Systematic Review. Front Immunol 10:856
Phetsouphanh C. et al. 2022. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol 23:210-216
Rheumatology Advisor. Exploring the Link Between COVID-19 and Autoimmunity Can Help Patients With Long-Haul COVID. Nov 5, 2021 https://www.rheumatologyadvisor.com/home/news/exploring-the-link-between-covid-19-and-autoimmunity-can-help-patients-with-long-haul-covid/
Merad M. et al. 2022. The immunology and immunopathology of COVID-19. Science 375:1122-1127
Hohberger B. et al. 2021. Case Report: Neutralization of Autoantibodies Targeting G-Protein-Coupled Receptors Improves Capillary Impairment and Fatigue Symptoms After COVID-19 Infection. Front Med(Lausanne) 8: 754667